Over the past 20 years, pharyngeal cancer has increased rapidly in the Western world, and some now refer to it as throat cancer. epidemic.
This is because a particular type of throat cancer called oropharyngeal cancer (the area of the tonsils and back of the throat) is on the rise significantly.
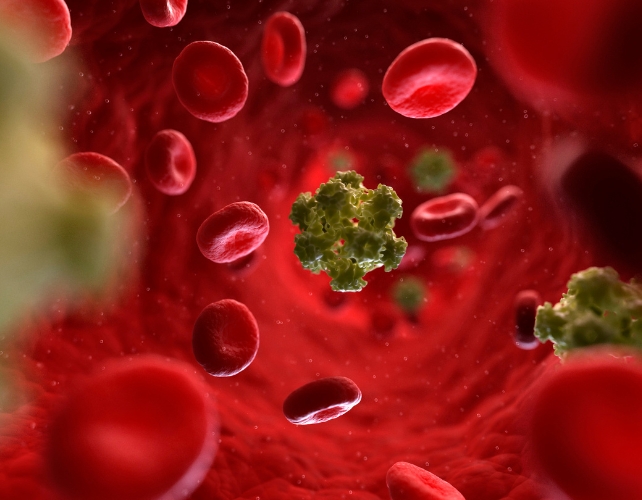
The main cause of this cancer is human papillomavirus (HPV), which is also the main cause of cervical cancer. Oropharyngeal cancer is now more common than cervical cancer in the US and UK.
HPV is transmitted through sexual activity. The main risk factor for oropharyngeal cancer is the number of lifetime sexual partners, especially oral sex. People who have had six or more oral sex partners in their lifetime 8.5 times They are more likely to develop oropharyngeal cancer than people who don’t have oral sex.
Research on behavioral trends shows that oral sex very prevalent in some countries. In a study my colleagues and I conducted of approximately 1,000 people in the UK who had tonsillectomies for reasons other than cancer, 80% of adults report having performed oral sex at some point in their lives.
However, fortunately, only a small number of people develop oropharyngeal cancer. It’s not clear why that is.
The general theory is that most of us can get an HPV infection and get rid of it completely. However, there are a small number of people who are unable to get rid of the infection, perhaps due to deficiencies in certain aspects of their immune system.
In these patients, the virus is able to continuously replicate and over time integrates into the host’s DNA at random locations, some of which can cause the host cell to become cancerous.
To prevent cervical cancer, HPV vaccination is being given to young girls in many countries. Not yet, but it is increasing indirect evidenceThis means that it may also be effective in preventing HPV infection in the mouth.
There is some evidence to suggest that juveniles are also protected as follows: “Herd immunity” in the countries Areas with high vaccination rates for girls (over 85%). Taken together, these may lead to a decline in oropharyngeal cancer in the coming decades.
This is all well and good from a public health perspective, but only if the prevalence among girls is high, at least 85%, and if one remains in the targeted “population.”
However, it does not guarantee protection at the individual level. Especially in this era of international travel, for example, if you have sex with someone from a country with low insurance coverage.
Certainly, countries with low vaccination rates for girls, e.g. Only 54.3% in the US Percentage of youth ages 13 to 15 who received two or three doses of HPV vaccine in 2020.
Boys should also receive the HPV vaccine
This has led several countries, including the United Kingdom, Australia, and the United States, to extend national recommendations for HPV vaccination to boys, known as gender-neutral vaccination policies.
However, even with a universal vaccination policy, coverage is not guaranteed. A significant proportion of the population opposes HPV vaccination due to concerns about safety, necessity, or, less commonly, concerns about encouraging promiscuity.
Paradoxically speaking, some evidence Population studies show that, perhaps to refrain from penetrative sex, young people may engage in oral sex instead, at least initially.
The coronavirus pandemic has also brought its own challenges. First, it has been impossible for some time to reach young people at school. Second, general vaccine hesitancy, or “anti-vaccine” attitudes, is increasing in many countries, which may also be contributing to the decline in vaccine uptake.
As always when dealing with populations and behavior, nothing is simple and straightforward.![]()
Hisham MehannaProfessor, Institute of Cancer and Genome Science University of Birmingham
This article is republished from conversation Under Creative Commons License. please read original article.
A previous version of this article was published in April 2023.







