Papovavirus is a term combining papillomavirus (PA), polyomavirus (PO), and vacuolating agent (VA). The name “papova” is derived from “papilla”, which refers to a bump, growth, or pimple, and “oma”, which means tumor. Historically, these viruses were divided into families. PapovaviridaeHowever, this classification is currently not recognized. Viruses are currently classified into two distinct families: human papillomaviruses (HPV) and human polyomaviruses.
- Papillomaviridae: Family of human papillomaviruses (HPV)
- Polyomaviridae: Family of human polyomaviruses
Vacuolating agents are also classified as: Polyomaviridae A family is a group of viruses that share certain characteristics. Papillomaviruses and polyomaviruses are both DNA viruses. naked viruswhich means the envelope is missing. This property makes them more stable in the environment and more susceptible to infection through direct or indirect contact.
Human papillomavirus (HPV)
human papillomavirus (HPV) is a group of more than 200 related viruses that primarily infect humans. skin mucous membranes of the genitals, mouth, throat, etc. HPV infection occurs in the following places: dividing epidermal cells or basal layer cells The area of the skin where the virus enters cells and begins replicating. HPV is very host specific and tissue specificThat is, they typically infect one species and target a specific type of tissue.
One of the challenges in HPV research is that HPV cannot be cultured in laboratory conditions. that Proliferates only within proliferating stratified squamous epithelial cellsare difficult to grow in vitro. This means that traditional cell culture methods for virus isolation are not applicable to HPV. the result, detection The rate of HPV infection is dependent on other techniques such as: immunoassay and gene probe.
HPV detection
Because HPV cannot be cultured, detection focuses on identifying the virus’ genetic material within infected cells. This can be done in a way like DNA hybridization (PCR, Southern blot hybridization) or in situ hybridization. mucosal smear Tests (cervical, vaginal, anal, etc.) are commonly used for testing. Pap smear test HPV testing is often included to detect the presence of HPV and identify the specific strain.
One notable limitation is that currently: There is no test that can detect HPV from male samples.. However, it is well established that men can also develop it. genital warts Although it is caused by HPV infection, the development of cancer is rare compared to women. Men are considered vectors of HPV transmission, including spread between Women who have sex with women (WSW).
Types of human papillomavirus HPV
HPV types are classified based on their properties. tissue orientationor prefer to infect certain types of tissues. HPV types are broadly classified into two groups.
- skin type: These mainly infect the skin and cause common warts.
- Type of mucous membrane: These infect the mucous membranes and are associated with: genital So are warts cervical cancer.
Among mucosal types, 40 types of HPV These are sexually transmitted diseases and are designated as: Types of reproductive organs. These types are further classified based on their association with: genital cancer As:
- High risk type: HPV 16, 18, 31, 33, 45, 56, 58, 59, and 68 are associated with an increased risk of: cervical cancer and other cancers.
- Low risk type: HPV 6 and 11 are mainly responsible for: genital warts It usually does not cause cancer.
- medium risk type: These types are associated with low-risk precancerous lesions, but are not as associated with cancer as the high-risk types.
Cervical cancer and HPV
One of the most significant medical concerns related to HPV is its strong association. cervical cancer. cervical cancer It is the third most common cancer in women worldwide. chest and colorectal cancer. It is mainly caused by infection with high-risk HPV types, especially HPV. 16 and 18responsible for approx. 98% of cervical cancers.
Actually, more than 50% of women contract a genital HPV infection within 2 years presumed to be sexually active 80% of women will be infected with HPV during their lifetime. However, most infections are temporary and asymptomatic, with no long-term effects as the body’s immune system clears the virus. In some cases, especially with high-risk HPV types, the infection can persist and lead to symptoms such as: Cervical intraepithelial neoplasia (CIN)which is a sign of cancer.
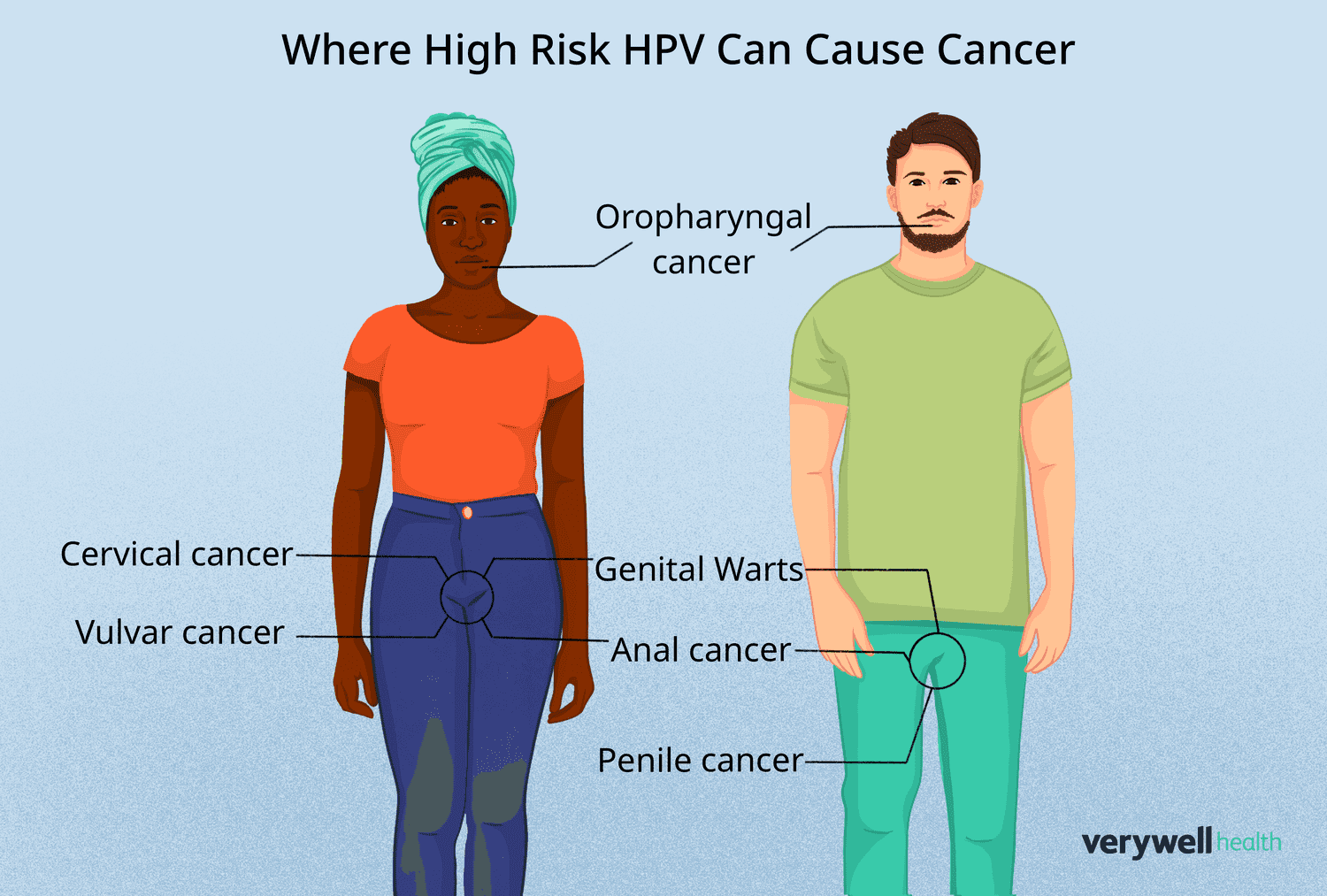
HPV and other cancers
meanwhile cervical cancer is the most well-known cancer associated with HPV, but other cancers are also associated with the virus. anal cancer It’s becoming more common, especially among men who have sex with men (MSM) and HIV-infected people. Although the incidence of anal cancer is still lower than that of cervical cancer, the incidence is increasing.
HPV can also cause cancer. oropharynxincluding throat, tonsiland tongueEspecially in individuals who perform oral sex. According to research, Oral and vaginal sex partnersshortage condom useand poor dental hygiene Correlated with increased risk of developing HPV-related oropharyngeal cancer.
Risk factors for cervical cancer
Several risk factors are associated with human papillomavirus infection and subsequent development of cervical cancer. These include:
- number of sexual partners: Women who have multiple sexual partners are at increased risk of contracting HPV.
- age of first sexual intercourse: Early initiation of sexual activity increases the risk of HPV exposure.
- male partner sexual activity: Male partners who have multiple sexual partners may increase the risk of HPV infection.
- Barrier contraceptive failure: Not using condoms increases the chance of HPV infection.
- smoking: Tobacco use weakens the immune system and increases susceptibility to persistent HPV infection.
- Oral contraceptive use: Long-term use of oral contraceptives may increase the risk of cervical cancer, especially in women who smoke.
- multiple pregnancy: Women who have had multiple pregnancies may have an increased risk of developing cervical cancer.
- immunosuppression: People with weakened immune systems, such as people with HIV, are more likely to develop persistent HPV infections.
HPV diagnosis
Diagnosis of HPV Infection often involves a combination of the following methods:
- Biopsy and histology: Examination of biopsy samples from abnormal tissue to identify changes characteristic of HPV infection.
- Papanicolaou (pap) smear: This is a widely used screening tool that involves collecting cells from the cervix. If HPV is suspected, additional tests are needed, including: DNA test (PCR, Southern blot hybridization) or in situ hybridization may be implemented.
Benign lesions caused by HPV
Many types of HPV infections can cause benign lesion Although it does not cause cancer, it can cause discomfort and cosmetic concerns. These include:
- common warts (Common warts): Characterized by a rough, raised surface, they are commonly found on the hands, knees, and feet.
- flat wart (Flat warts): Smoother and flatter than common warts and usually seen in children.
- Butcher’s Words: Associated with butchering, but why they occur in this profession is not fully understood.
- genital warts (Warts acuminata): Caused by HPV types 6 and 11, these warts are found in the genital and anal areas. Although usually benign, it can cause discomfort and complications during childbirth.
Malignant or potentially malignant lesions
HPV can also cause symptoms such as Malignant or potentially malignant lesionsinclude:
- Bowen-like papulosis: resembling papules on the penis or vulva bowen disease. These lesions can eventually become malignant.
- Intraepithelial dysplasia: Abnormal changes in the epithelium of the cervix. Commonly referred to as CIN (cervical intraepithelial neoplasia). Vain (vaginal intraepithelial neoplasia), and VIN (vulvar intraepithelial neoplasia). CIN 3, the most severe form of dysplasia, affects all layers of the epithelium and is more likely to progress to invasive cancer.
Vaccination and prevention
The best way to prevent HPV-related diseases is to vaccination. The HPV vaccine is most effective when given before you start having sex. of CDC The HPV vaccine is recommended for people of the following ages: 11-12 (However, vaccinations can begin at age 9). a 3-dose regimen Typically used as follows:
- Initial dose: This will be given to you at your first visit.
- second dose: 1 to 2 months after the first administration.
- 3rd dose: 2 months after the second vaccination.
The available vaccines are:
- 2vHPV (Cervarix): Targets HPV 16 and 18 (approved for women only).
- 4vHPV (Gardasil): Targets HPV types 6, 11, 16, and 18 (approved for both men and women).
- 9vHPV (Gardasil-9): Targets 9 HPV types (6, 11, 16, 18, 31, 33, 45, 52, 58) and can be used for both men and women.
These vaccines are preventiveThat is, it prevents infections but does not treat existing infections.
treatment and management
at present, antiviral drugs It can be used to treat HPV infections. Vaccines provide protection against infection pre-cancer There are non-invasive cancers, such as pre-cancer of the cervix, but active infections cannot be cured. HPV-related treatments wart Lesions often require local treatment, cryotherapy, or surgical excision.
conclusion
Human papillomavirus (HPV) infection is a global public health problem and contributes significantly to the development of cancers such as cervical cancer. There is no cure for existing HPV infection, but you should take the following precautions: vaccination Shown to reduce the incidence of HPV-related cancers. Comprehensive education, early detection, and vaccination are essential to reduce the burden of HPV on public health.







